Digital health governance in China by a whole-of-society approach
In the context of the global digital transformation, the health sector is receiving unprecedented attention. In order to advance digital health, the World Health Organization has launched a series of policies, including the Global Strategy on Digital Health 2020–20258. This strategy places governance at the core, aiming to enhance the necessary capabilities and competencies for countries to advance, innovate, and disseminate digital health technologies, and ultimately contribute to universal health coverage. However, the implementation of these principles is deeply shaped by the specific local governance structures and contexts. This study analyzes China’s policies and practices, and maps the architecture of digital health governance within the country. Findings from this study offer valuable insights into governance structures that can facilitate digital transformation and could serve as an example for other low- and middle-income countries (LMICs) to navigate similar challenges in digital health transformation.
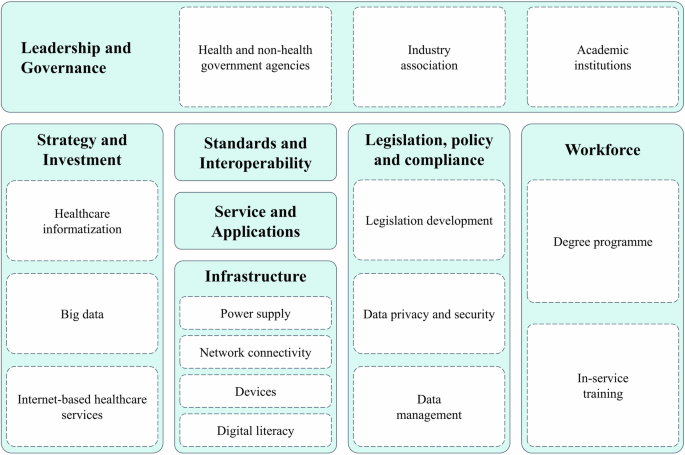
China’s governance structure for digital health is supported by political commitment, cross-sectoral collaboration, and a whole-of-society approach. The State Council has issued overarching strategies, including the Guiding Opinions on Promoting and Regulating the Development of Big Data Applications in Healthcare17 (2016) and the Opinions of the General Office of the State Council on Promoting the Development of Internet Plus Health Care10 (2018). A multi-sectoral cooperation mechanism has been established, comprising 12 ministries and commissions, including those health-related sectors (e.g., the National Health Commission, State Administration of Traditional Chinese Medicine, and National Healthcare Security Administration) as well as cross-cutting sectors that play a pivotal role in digital health functions. Moreover, academic institutions and private sectors like industry associations play an active role in governance, reinforcing a whole-of-society approach to digital health transformation. Their participation reinforces the whole-of-society approach to digital health transformation, ensuring that a broad range of stakeholders contribute to the ongoing development and regulation of digital health technologies. A key driver of this transformation is the development of digital and physical infrastructure—the first level of the digital divide. Disparities at this level create a cascading effect: limited internet access in rural areas not only hampers connectivity but also reduces digital literacy (second level) and limits the use of digital health services like telemedicine and remote monitoring (third level). This layered divide risks widening health disparities between urban and rural populations, highlighting an infrastructure gap in China that warrants attention for other LMICs.
Notwithstanding the progress, the fragmentation of data remains a foundational obstacle and has emerged as a priority for the next step. While informatization efforts began as early as 2002, the issue of “information silos” continues to hinder progress. The use of vertical, standalone ICT solutions has led to isolated systems that fail to communicate with one another, preventing access to the full spectrum of relevant health information. At the provincial level, efforts are being made to address these issues. For example, the Beijing Health Commission’s 2024 work plan prioritizes the integration of health data across a network of more than 170 hospitals in the city54. This approach is intended to connect various data sources and create a more unified system for healthcare information. Health insurance data is seen as a central element in this integration effort, serving as a crucial link that can connect healthcare service documents across different platforms. To further enhance data integration, a more comprehensive approach is needed. This would involve not only hospitals and healthcare centers but also primary care providers, public health programs, insurance reimbursement systems, and personal health data from wearable devices, to enable a more connected and efficient healthcare ecosystem to support better decision-making and health outcomes.
Motivating the data integration requires a strong focus on privacy protection and security55. Innovative solutions, such as privacy-preserving computing, have been proposed. Privacy-preserving computing, using technologies like secure multi-party computation, federated learning, and trusted execution environments, enables secure data sharing while maintaining privacy. These technologies allow computations on encrypted data, ensuring privacy during integration and analysis. Since 2023, the Suzhou Health Commission has developed a secure platform for medical data sharing, utilizing privacy-preserving technologies. The platform enables secure sharing of demographic data, EHRs, health knowledge, and public health records, enhancing data security, regulatory effectiveness, and healthcare standards56.
Policies gain significance only when effectively translated into practice. To evaluate the effectiveness of policy implementation across different regions, China has conducted the National Healthcare Information Standardization Maturity Measurement Program since 2020. This program evaluated the informatization capabilities of participating regions and hospitals through technical assessments23. Utilizing the National Health Informatization Development Index57, the program comprehensively measures cities across three key dimensions: governance capacity, infrastructure development, and application efficacy. The results highlight significant progress in China’s health informatization efforts, showcasing advancements in organizational frameworks, foundational infrastructure, and improved collaboration mechanisms among healthcare institutions. Moreover, the findings indicate increased maturity in data sharing and exchange, reflecting enhanced interoperability within the healthcare system.
Tailored governance models were observed across provinces and regions. In resource-rich areas, local health authorities build regional health information platforms through a bottom-up integration of medical data from all levels of healthcare institutions. Resource-scarce regions adopt a top-down approach, where large hospitals collaborate with a limited number of primary care facilities to provide support and foster regional medical cooperation58. For example, Zhejiang Province, which has the leading GDP per capita across China, focused on efficient healthcare services and life-course health management by utilizing digital platforms like Digital Health Angel, Zhejiang Medical Mutual Recognition, and Zhejiang Nursing59. Qinghai Province, located in the western part of China, addresses the accessibility challenges posed by its vast geographical landscape by offering telemedicine. This includes the establishment of a four-tier remote medical service system that connects provincial, municipal, county, and grassroots levels, thus improving healthcare access in the region60.
The adoption and utilization of healthcare providers and the general population are also essential for the digital transformation. To promote the utilization of healthcare providers, especially in low- and middle-income countries, it is critical to establish supportive infrastructure, provide tailored training, and implement incentive policies that foster a conducive environment for their adoption61. For the general public, while digital health technologies are becoming more common, there are still several challenges. These include issues with usability, concerns about security and privacy, a lack of industry standards, and various technical problems37,62. Further monitoring and evaluation are needed, from the perspective of digital health users, to further provide a supporting ecosystem for the digital transformation.
In the era of digital transformation, China’s governance structure and experience can offer useful lessons for other LMICs. Digital health has great potential to make health systems more efficient and sustainable. It can also help provide better care across different situations and for various population needs. However, many LMICs struggle with weak governance that does not align with the core Health for All values63. There is a need to move beyond the current focus on project-based, externally funded, and isolated efforts and instead drive digital transformation to build sustainable and integrated digital health systems. China’s experience highlights key elements for digital health governance: (1) a clear national strategy and a way to coordinate between government bodies and other groups; (2) basic infrastructure, such as power, network connections, devices, and digital skills; (3) strong focus on privacy and data security through laws and new technology; (4) training programs to improve digital skills for healthcare workers and vulnerable groups; and (5) strategies that are adapted to the local situation and development stage. It is important to understand that there is no “one-size-fits-all” approach for digital health governance. Each country will need a tailored structure and strategy, based on its health system, government, and the role of the private sector.
In summary, this study systematically examined digital health governance in China, and highlighted policy arrangements, implementations, challenges, and the path forward. The whole-of-society approach to digital transformation in health systems offers a valuable example and policy insights for other LMICs in promoting digital transformation based on the Health for All values and adapting to local contexts.
link




:max_bytes(150000):strip_icc()/longhair-cat-window-1221937516-2000-6b9bf7aaff7742539005c0b08593f856.jpg)